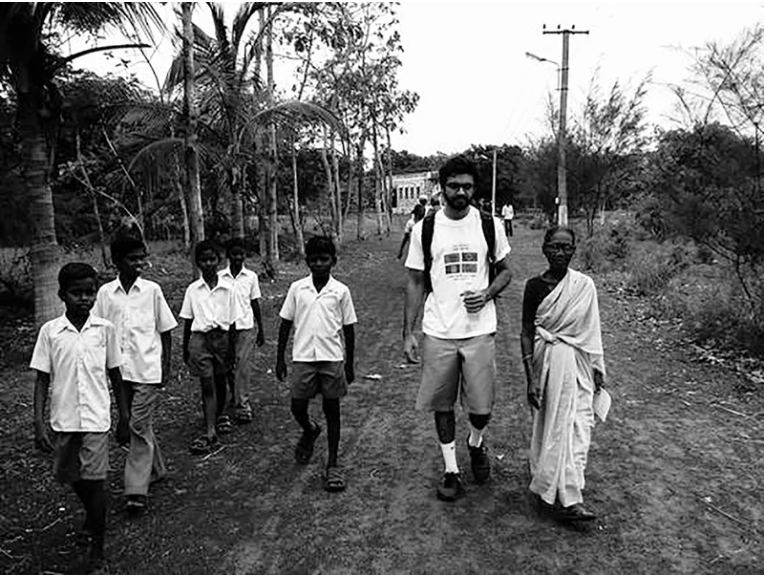
On a trip to India, Abraar Karan (second from right) interviews a local woman to talk about the challenges of cataracts.
Daniel Carvalho
"Any western medical institution more than a century old and which claims to stand for peace and justice has to confront a painful truth — that its success was built on the savage legacy of colonialism."
Richard Horton, editor of The Lancet, wrote this bold indictment in a column in the journal this year.
To young Western doctors working in poor communities, no more important words could be heard.
Today, the field of "global health" strives to create equitable and just relationships between wealthy and impoverished regions, places and peoples. But it is still a field with markedly unequal power dynamics: racism, classism and many of the residual exploitations of a terrible colonial past. I fear that this point often goes missed or ignored, possibly because we are subconsciously or consciously engaged in a neocolonial narrative in which wealthy people are "saving" poor people even as they build their own careers.
It is not a relationship in which Western visitors and local people are collaborating equally — or perhaps even more appropriately, where local leaders take the dominant role.
I recently completed a global health course. There were lectures on AIDS, malaria and tuberculosis treatment and on noncommunicable diseases such as diabetes and hypertension in Africa.
But not one of these discussions addressed the remnants of colonial mentality. If anything, that mentality was pervasive in the academic framework. Most of the lecturers were from high-income countries as were most of the students, including myself.
Yet our discussions were largely about other people in other countries, most of which had been colonies in the past. I could not help but think that there should have been more people from the countries we were talking about both on the stage and in the seats.
First, do no harm
If you are from a high-income country working in a low-income setting, and you don't think and rethink about this topic often, there is a good chance you are contributing to the problem.
Admittedly, I know that I have contributed to it. As a college student, I participated in a volunteer trip to the Dominican Republic in 2008 — my first experience with international health.
I was a Spanish translator for American doctors seeking to create a program with the local community. This was meant to become a long-standing annual trip for medical and public health work — including potentially creating a permanent clinic where alumni could come to work.
But this project was not continued after our two-week "parachute-trip." Logistical issues precluded us from forming a longer, more meaningful connection. But now as I look back, I recognize that this project certainly connected to themes from the colonial era: Western doctors traveling to unknown territories to help less-educated locals.
That experience made me realize how problematic short-term trips could be and steered me into a career in global health as a way to make a sustained contribution to the field rather than just dropping in for quick missions.
Back in 2008, on one of our many evening drives home in the back of flatbed trucks through the Dominican countryside, I remember a candid discussion with one of the doctors. We lamented that even though we were working to treat coughs, colds, diarrhea and fevers, we were doing nothing to treat all of the reasons contributing to these diseases: poverty, the lack of paved roads and latrines, food insecurity, insufficient education and even political disenfranchisement — if you're not able to vote in fair elections, how can you hope to have any impact on government health care decisions?
A drop-in medical mission trip certainly was not the way to solve these problems. While the local people had a continual struggle against poverty, we as the Western visitors had the luxury of leaving whenever we wanted.
They also had no recourse against us if we were to behave inappropriately — no way to hold us accountable. There was nothing they could do about the group of foreigners who came, saw and ultimately did not stay or return.
Certainly those of us working on the program were better than brutal colonizers. But were we that different in the very basic power dynamics between light and dark skin? Between wealthy and poor? Moreover, the nature of our mission perhaps confirmed the worst fears of the local community: We would not be coming back there.
Many times, we were asked when we would return, but most of us knew that the answer was at best uncertain. So we only vaguely could respond with "en el futuro" — in the future.
And admittedly, I benefited: In 2008, having a global health experience on your CV was a big deal. Today, I feel guilt that I benefited because of it, even if that was not my primary reason for being there. At that time, I really did not know what I wanted to do with my career, and this was an opportunity to see if it might be global health care.
Dismantling our own power
Having reflected on the harm that we from the West have caused, I'm now asking the obvious question: What can we do about it?
Even if you have never worked in global health, the color of your skin and the accent of your voice may unduly confer upon you a level of authority in poor communities that you likely do not deserve and should not have. This is a symptom of inequity that calls upon all of us in this seat of privilege to dismantle our own power — to push back against colonial legacy with humility; to say to yourself, your colleagues, and the people you are working with: "We are not experts here; we are the students."
Furthermore, the relationships within global health are still heavily (and falsely) dominated by the idea that the Global North is "helping" the Global South. The opposite is rarely acknowledged or encouraged in any meaningful way. Even when doctors from impoverished countries are brought to wealthy countries as part of exchange programs, it is under the assumption that they are coming to learn from us.
This is, of course, not true. Much of what I have learned has been from the wisdom, ingenuity and perseverance of doctors and other health care staff who live and work in low-income settings. From them, I have learned how to rely on a physical exam rather than expensive and overutilized technology.
I've also become more sensitive and aware of the challenges suffered by my underserved patients in the U.S. For instance, the same challenges that my patients in sub-Saharan Africa faced are commonly shared by patients I see in my predominantly Latin American clinic in Boston. They cannot afford or find healthy foods, they lack disposable income for convenient transportation to a medical center, and for many, English is not a first language, if they can speak it at all. When a patient of mine misses an appointment, I call to figure out why.
I do not write this to say that there is no role for doctors from high-income places to work in global health. There certainly is, and in fact, it is more than a role. It is a responsibility. Part of the legacy and inequity of colonialism is that we in the Global North benefit from access to new technologies, drugs, equipment and money as well as sanitation, electricity, transportation. The list goes on.
But that is not because we are any better than doctors in poor countries. It is because our leaders have collectively and systematically done everything possible to make sure those countries stayed less economically empowered than our own for centuries.
Our role in global health as practitioners from wealthy countries is then not a practice in which we are "helping" poor countries; it is one in which we are hoping they can forgive us for having decimated them in the first place.
In the 1899 poem, The White Man's Burden, the English poet Rudyard Kipling talks about what he sees as the responsibility of wealthy countries to help poor countries as the burden placed upon the white man. In response, a black clergyman, H.T. Johnson, wrote a piece, The Black Man's Burden just a few months later. He rightly points out that the burden is the other way around — that actually, black and brown people have suffered the burden of white colonialism and imperialism, forces that have not helped them but exploited and killed them.
Today, the same holds true, just repackaged. The burden is carried by black and brown people (as well as poor white people from disenfranchised groups) because of the ills of a still-thriving imperialist white dominance.
We see this burden in global health research, which is still largely dominated by Western researchers building their careers off studies of vulnerable, marginalized groups who often don't understand their roles or participation.
We see this in pandemic disease response, which has been disruptive to local cultural and health systems (Ebola, for instance, pulled many financial and operational resources away from other health and human rights maladies in the Congo that are killing even more Congolese).
We see this in short-term global health trips, which help students from Western institutions gain "experience" at the expense of poor people in faraway places.
Certainly not all is bad in global health, but the bad seems to be far less talked about than the good.
At its worst, global health today is a self-congratulatory neocolonial machine in which doctors, professors, researchers and others from wealthy places with abounding privilege are further exalted because they are doing work that their Global South counterparts do as part of their everyday lives with little to no recognition. At its best, it is a humble attempt to equal the playing field of life between North and South by trying to unravel the tightly bound chains of colonialism.
I'm now a physician at Harvard University and Brigham and Women's Hospital with a strong record of long-term global health partnerships. Our programs have a particular emphasis on establishing human relationships and building, empowering and supporting local health leaders as central tenets of the work. One example of this is the University of Global Health Equity, a medical and public health school in Rwanda with a focus on training African students to become leaders in global health and to lead health care efforts in their home countries.
From many of the impoverished patients I have worked with, I have learned that the challenges that help a Western doctor build a career or feel altruistic are the harsh never-ending realities of their life — every day, every year, from birth until death. When we fail to recognize this harsh truth, we end up taking our power for granted. There is nothing more dangerous than that.
Abraar Karan is an internal medicine resident in the Hiatt Residency in Global Health Equity at Brigham and Women's Hospital and Harvard Medical School. All views expressed are personal and do not represent those of any listed institutions. You can contact the author via Twitter @AbraarKaran
Your Turn
Have you taken part in a global health program in a developing country? Has that program taken any recent steps to give power to local medical professionals? Share your story in an email to goatsandsoda@npr.org with the subject line "global health programs." We are taking responses until Jan. 7. We may reach out to you if we are interested in including your story in a future article.
Poster un Commentaire