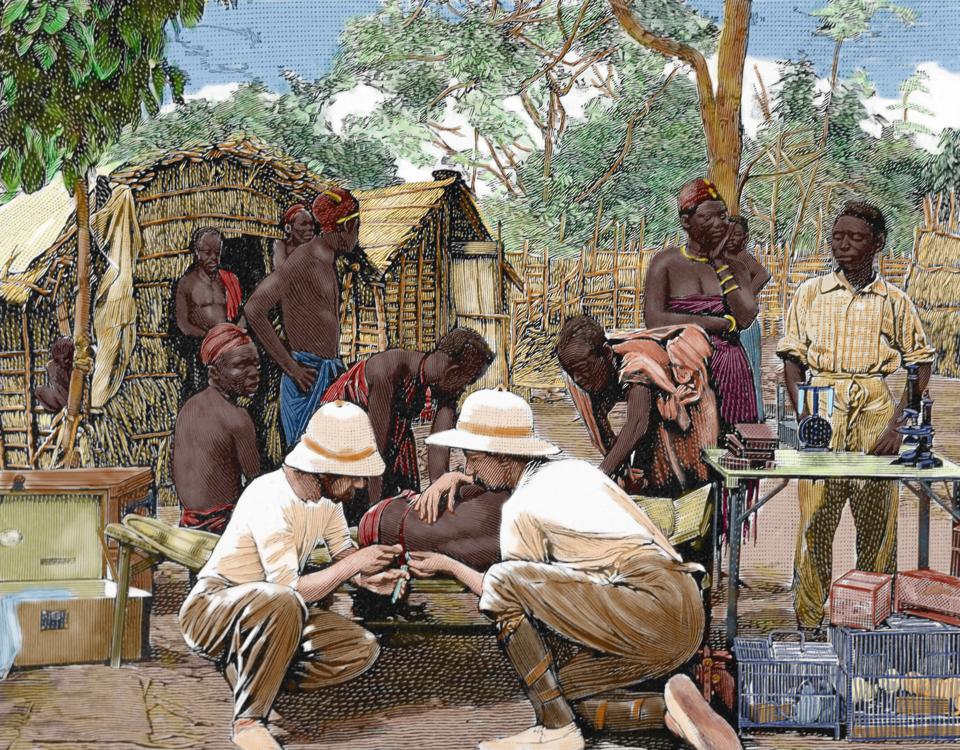
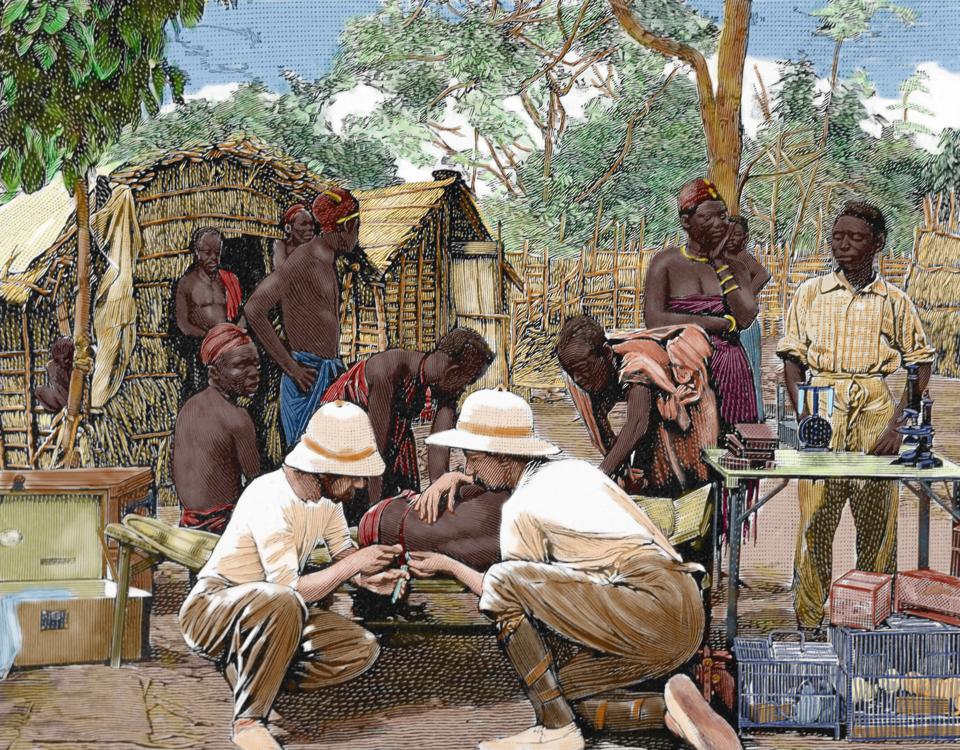
HISTORY OF AFRICA, Doctors in an expedition of European explorers, examining the native blood attacked by sleeping sickness, Engraving by Thiriat, 1903, Colored. (Photo by Prisma/UIG/Getty Images) UNIVERSAL IMAGES GROUP VIA GETTY IMAGES
During the 1990s, I was doing my medical training in India. Those days, we had a steady stream of American and European students visiting our medical school. They would stay for a few weeks, work on short-term projects, and go back home to publish their research in international journals. None of us got to publish much, despite the fact that we (the locals) had lived experience in dealing with the problems under study, and had deeper insights than our visitors could have gained in a few weeks.
Have we come a long way since my training days? Not quite. Research shows that global health is still struggling to shed its colonial past. This is reflected in who drives the research agenda, who dominates authorship, and who edits the research.
Who is driving the research agenda?
The global health research agenda is driven largely by funders (e.g. US NIH, Bill & Melinda Gates Foundation, Wellcome Trust), major global health agencies (e.g. WHO, World Bank, USAID, Global Fund, US CDC, and universities). Nearly all of these are led or dominated by experts from the Global North. They set and drive the research agenda, on behalf of people in low- and middle-income countries (LMICs).
Take tuberculosis (TB), for example. TB is primary a problem of LMICs, but TB research funding and publication output is dominated by the United States (which has a very low incidence of TB).
Who is publishing the research?
There is growing awareness about 'safari or parachute research' and its negative consequences. The recent story of Jean-Jacques Muyembe, the Congolese doctor who discovered Ebola but did not get much credit until today, is a striking but perhaps extreme example.
But even when research is done collaboratively, there are issues with authorship and inclusion. In an analysis of research studies conducted in Africa on HIV, malaria, TB, salmonellosis, Ebola and Buruli ulcer, Mbaye and colleagues found that African authors are highly under-represented as first and last authors (authorship positions that often get the most visibility and credit).
In a similar analysis, Hedt-Gauthier and colleagues found that over 50% of all coauthors and of first authors on papers about health in Africa were from the country of the paper’s focus. However, if any coauthors were from the USA, Canada or Europe, then overall representation of African authors dropped, particularly in the first and last author positions. This was most frequent when collaborators were from an American university.
Trends from specific global health journals (e.g. Lancet Global Health), and specific areas of research (e.g. pediatrics, maternal health) confirm these findings of under-representation of authors from LMICs.
Who is editing the research?
Since editors act as gatekeepers, who edits research matters a lot. In a recent study, we examined the composition of editors and editorial board members of 12 major global health journals to examine diversity and inclusion. Across all journals, only a third of editors were female, and a third were based in LMICs. Only 1 in 10 editors were women based in LMICs. Among the 12 journals, all except two were managed by institutions in USA or Europe.
A more expanded analysis of 27 specialty global health journals by Bhaumik and Jagnoor showed that 60% of the editors were men and 70% were based in high-income countries. All but one of the 27 journals were published in high-income countries.
Given these findings, it is easy to understand why research papers from LMICs, written entirely by local experts, rarely get published in high-impact journals.
Unpacking and tackling inequities
Equity is at the heart of global health. And yet, as shown by these research studies, global health researchers, funders and journals are not walking the talk on equity, diversity and inclusion.
Some of the concerns (e.g. editorial board diversity) can be addressed quickly. Indeed, some journals (e.g. Lancet Global Health, BMJ Global Health) have already pledged to achieve parity in gender and representation of LMIC expertise. I hope other global health journals will follow suit.
But there are deeper layers to the problem and addressing them will require much more than the reconfiguration of editorial boards. It will require us to collectively ask and address hard questions such as, why, in 2019, most global health journals and funders are headquartered in London, New York, Geneva, and Seattle, and run by colonial-era institutions?
In this context, Seye Abimbola, editor of BMJ Global Health, has written an important piece called "The Foreign Gaze," where he attempts to unpack the imbalances in academic global health.
Abimbola begins by quoting Toni Morrison, who wrote: “Our lives have no meaning, no depth without the white gaze. And I have spent my entire writing life trying to make sure that the white gaze was not the dominant one in any of my books.” By rejecting the "white gaze", Ms Morrison helped black people see themselves in their own stories.
According to Abimbola, there is a similar problem of gaze at the heart of academic global health. He prefers to replace the word ‘white’ with the word ‘foreign’.
"The growing concerns about unfair distribution of authorship are really about unequal distribution of power in global health, power to determine which questions are worth answering, who the audience of those answers really are, and how those answers are published."
According to Abimbola, our efforts to address imbalances in authorship in global health are incomplete without aiming to go beyond mere representation on lists of authors; without tackling the colonial attitudes and practices that those imbalances represent.
His paper shows that those colonial attitudes and practices manifest in three important ways:
1. foreign experts who write about local issues without acknowledging how and why their real audience is actually not local experts, but other foreign experts.
2. foreign experts who set out to write for an audience of local experts without acknowledging the limitations of what they can possibly know about local realities.
3. local experts who write for a foreign audience, without acknowledging how that imagined audience influences what they study and what they write.
"It is very easy to submit to the colonial conditioning of global health. So, it is important that we become more aware of these often subtle, but consequential choices we make as authors, and feel free enough to talk about them in the open," he says.
As I read Abimbola's insightful paper, I finally understood my own frustrations with the foreign gaze during my training days in India. I think I felt that local experts were undervalued and rarely got a chance to display their expertise on the international stage.
Today, I am a "foreign expert" living in Canada. I understand that I need to be more reflective on the choices I make, and "lean back" when the situation does not demand a foreign gaze, or when a foreign gaze can actually be a barrier to making real progress on the ground.
Acknowledgement: I am grateful to Dr Seye Abimbola, School of Public Health, University of Sydney, for his encouragement and feedback.
Disclosure: I have no financial conflicts. I serve on the editorial boards of BMJ Global Health, and Journal of Epidemiology & Global Health.
Poster un Commentaire